Did you know nearly 70% of women with Polycystic Ovary Syndrome (PCOS) have endometrial issues? This fact highlights how important endometrial health is for managing PCOS. Women with this hormonal disorder may encounter several challenges for their uterine health.
It’s crucial to understand this link because hormonal imbalances can lead to conditions like endometriosis and uterine fibroids. By knowing about these concerns, women can take steps to manage their health better. Making informed choices is key to improving well-being when dealing with endometrial health and PCOS.
Key Takeaways
- PCOS significantly impacts endometrial health, with a high prevalence of related concerns.
- Understanding hormonal imbalances is crucial for effectively managing symptoms.
- Proactive health measures can help mitigate the risks associated with endometriosis.
- A well-informed approach to uterine health can enhance overall wellness.
- Regular screenings are essential for identifying and addressing endometrial issues early.
Understanding PCOS and Its Impact on Women’s Health
Polycystic ovary syndrome (PCOS) is a hormonal disorder affecting many women. The PCOS definition includes symptoms like irregular periods, excessive hair growth, and weight issues. It’s a major concern in women’s health, affecting millions worldwide.
The impact of PCOS goes beyond just reproductive health. It’s linked to metabolic syndrome and type 2 diabetes due to hormonal imbalances. These issues increase the risk of serious health problems. Furthermore, PCOS can lead to emotional and mental health issues, such as anxiety and depression.
Understanding the link between PCOS and reproductive disorders is crucial. Hormonal irregularities can affect endometrial health. This impacts overall well-being and fertility.
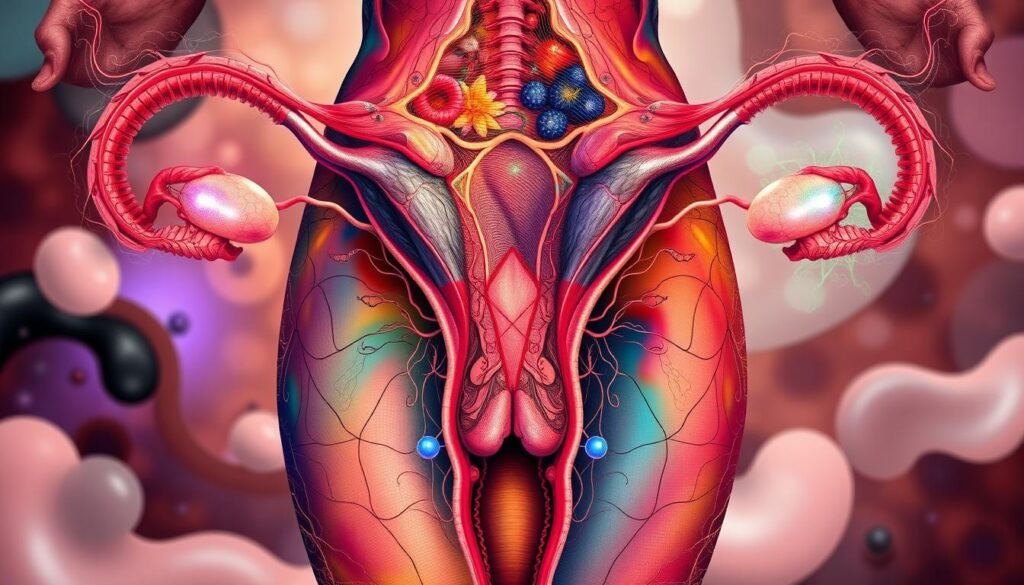
What is Endometrial Health?
Endometrial health is about the state and performance of the uterus’s inner layer. It’s key to know how this tissue is linked to reproduction, like egg attachment and periods. Healthy endometrium matters for both fertility and overall health.
Importance of a Healthy Endometrium
Keeping the endometrium healthy is very important. A functional endometrium helps with embryo implantation and pregnancy maintenance. Poor endometrial health might cause reproductive problems, including infertility and unusual bleeding. Women, particularly those with PCOS, should regularly check their endometrial health.
Factors Affecting Endometrial Health
Many things can affect endometrial health. These include:
- Hormonal levels: Hormones like estrogen and progesterone keep the endometrial lining healthy.
- Age: Hormonal changes from aging can harm endometrial health.
- Lifestyle: Diet, exercise, and stress levels affect reproductive health overall.
- Medical conditions: Issues like PCOS, endometriosis, and fibroids can interfere with endometrial function.
Knowing these factors helps women care for their endometrial health better. They can take steps for good reproductive health.
Identifying Common Endometrial Concerns
Knowing the signs of endometrial issues is vital for women’s health, especially for those with hormonal imbalances. Spotting these signs early on can help secure timely medical care. This can improve health results significantly.
Signs of Endometrial Issues
Signs to watch for include:
- Changes in menstrual patterns, such as irregular cycles
- Pelvic pain that may occur during menstruation
- Heavy or prolonged bleeding
- Abnormal spotting between periods
These signs could point to several endometrial problems. Seeing a doctor for these issues is crucial for good care.
Role of Hormonal Imbalances in Endometrial Health
Hormonal imbalances can deeply affect endometrial health. For example, PCOS causes hormone levels to fluctuate. This can mess up the menstrual cycle and worsen endometrial symptoms. Handling these imbalances is key for better health.
Knowing how hormonal imbalances and endometrial health are linked is important. Women looking to better their health should learn about these factors. To get more info on understanding and managing PCOS, check out this resource.
Endometriosis and Its Connection to PCOS
Endometriosis is a health issue that many women face, especially those showing signs of PCOS. By looking at its link to PCOS, we can see how they might impact each other and make it harder to manage one’s health. It’s often linked with continuous pelvic pain and painful periods, so it’s crucial to recognize these signs early on.
Symptoms of Endometriosis
Endometriosis can bring about a variety of symptoms with varying levels of discomfort. Key symptoms often include:
- Chronic pelvic pain
- Painful periods
- Pain during intercourse
- Menstrual irregularities
- Gastrointestinal issues
These symptoms might be more intense for women with PCOS, leading to a more challenging situation that needs close watch and care.
Diagnosis and Treatment Options
It’s very important to correctly diagnose endometriosis for proper treatment. Doctors use various ways to diagnose, including:
- Pelvic exams
- Ultrasounds
- Laparoscopy
Each method helps in understanding the severity of endometriosis and designing a suitable treatment strategy. Treatment options include:
| Treatment Type | Description |
|---|---|
| Medication | Pain relievers, hormonal therapies. |
| Surgery | Removal of endometrial tissue and adhesions. |
| Physical Therapy | Techniques to alleviate pain and improve pelvic function. |
Knowing the connection between endometriosis and PCOS helps women seek the right help. This way, they can get the most effective treatment possible.
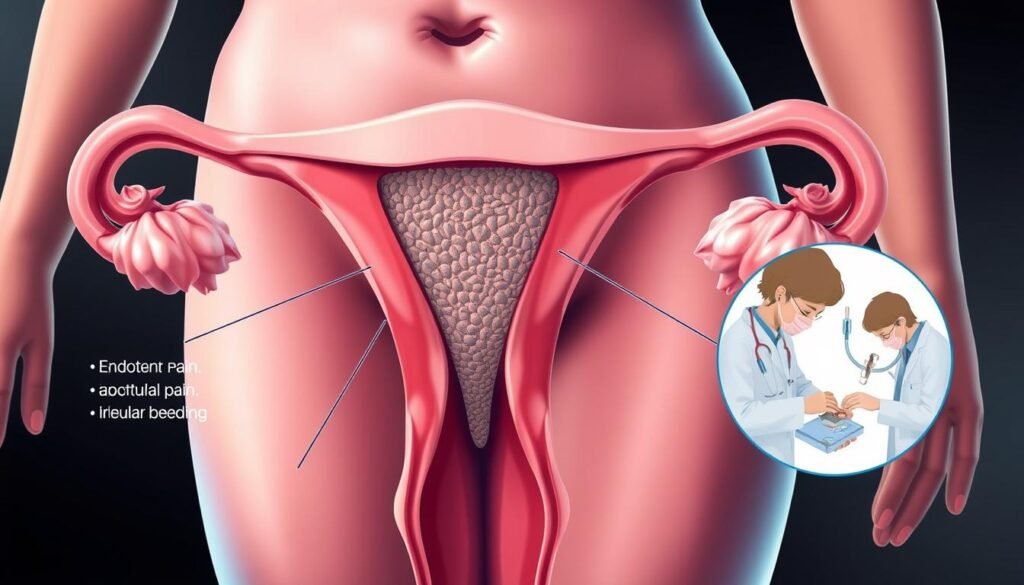
Uterine Fibroids: Risks and Symptoms
Uterine fibroids are non-cancerous growths inside the uterus. Knowing the risks and symptoms is key for women with reproductive health issues. Uterine fibroids symptoms include heavy bleeding, pelvic pain, and belly pressure. While some women don’t feel these, others find their lives greatly affected.
Understanding Uterine Fibroid Development
Many factors lead to uterine fibroids. This includes genetics, hormone levels, and growth factors. Women with fibroid family history face a higher risk. Being overweight or early menstruation also boosts fibroid growth chances. Knowing these risks helps catch them early for fibroid treatment.
Managing Fibroid Symptoms with PCOS
Women with PCOS find uterine fibroids especially challenging. PCOS causes hormonal imbalances that can worsen uterine fibroids symptoms. Managing PCOS well can help. Lifestyle changes like diet and exercise improve hormones and may ease symptoms. Some need medicine or surgery. Talking to specialists in PCOS and fibroids helps craft the best care plan, improving health.
Abnormal Uterine Bleeding: Understanding Causes
Many factors can cause abnormal uterine bleeding. It’s a significant concern for women’s health. Knowing why it happens is key to dealing with it. This section looks at what might cause it and how PCOS affects bleeding.
Potential Triggers of Abnormal Uterine Bleeding
There are several reasons for abnormal uterine bleeding. Here are some common ones:
- Hormonal imbalances, such as those from menopause or thyroid issues.
- Structural problems like uterine fibroids or polyps.
- Some medicines, like anticoagulants and hormone treatments.
- Stress and big changes in life, affecting hormone levels.
- Diseases like diabetes or liver problems.
Link Between PCOS and Abnormal Bleeding Patterns
PCOS can cause unusual bleeding, which is hard to figure out. Women with PCOS might see:
- Irregular periods, making bleeding unpredictable.
- Heavy or long-lasting periods due to hormone changes.
- Bleeding between periods, which can worry them.
Getting to know these PCOS bleeding patterns is crucial. It helps in diagnosing and finding the right treatment. If you notice these signs, get medical help to discuss what you can do.
| Trigger | Description |
|---|---|
| Hormonal Imbalances | Hormone levels off balance, causing irregular or heavy bleeding. |
| Structural Abnormalities | Issues like fibroids or polyps leading to atypical bleeding. |
| Medications | Drugs that change the flow and consistency of menstrual bleeding. |
| Stress | Stress, whether emotional or physical, might cause unusual bleeding. |
| Underlying Conditions | Long-term health issues affecting reproductive health. |
Exploring Endometrial Hyperplasia
Endometrial hyperplasia involves the uterus’s inner lining becoming thicker. It’s often caused by hormone imbalances, where there’s a lot of estrogen and not enough progesterone. It’s important to catch this early. If not, it could lead to cancer.
What is Endometrial Hyperplasia?
This condition can show up in different ways. Some types are simple, some are complex, and some have atypia, meaning abnormal cells are present. Atypical hyperplasia means there’s a higher chance of it turning into cancer. That’s why keeping an eye on it is crucial for women’s health.
Risk Factors for Developing Hyperplasia
Knowing what increases the risk of endometrial hyperplasia helps in catching it early. Here are some common risk factors:
- Obesity: Extra body fat can increase estrogen levels, raising the risk of hyperplasia.
- Age: Women over 50 are more susceptible due to hormonal changes during menopause.
- Long-term estrogen therapy: Unopposed estrogen therapy without progesterone can lead to an imbalance.
- Polycystic ovary syndrome (PCOS): This condition is associated with irregular menstrual cycles and estrogen excess.
Being aware of what causes endometrial hyperplasia and its risks can lead women to get the right help. This knowledge is powerful for prevention and treatment.
| Risk Factor | Description |
|---|---|
| Obesity | Excess fat tissue can lead to increased estrogen production. |
| Age | Higher risk in women over 50 due to hormonal shifts. |
| Estrogen Therapy | Unopposed therapy raises estrogen levels without balancing progesterone. |
| PCOS | Associated with hormonal imbalances and irregular cycles. |
Endometrial Polyps and Their Implications
Endometrial polyps are growths in the uterus lining. They range in size and number. You might see symptoms like irregular bleeding, or heavy periods. Or, you might not notice anything unusual. It’s hard to spot these polyps without a doctor’s help.
These polyps can impact a woman’s health in various ways. They may affect fertility and increase the risk of pregnancy problems. They can also make miscarriage more likely. It’s important to keep an eye on them and get the right medical care.
Different treatments exist for these polyps. Removal through surgery, like hysteroscopy, is common for those with symptoms or trying to get pregnant. Hormonal therapies might also help. It’s best to talk to a doctor to find what works for you.
| Type of Treatment | Description |
|---|---|
| Hysteroscopy | A minimally invasive procedure to remove polyps through the cervix. |
| Curettage | A surgical scraping of the uterine lining to remove polyps and abnormal tissue. |
| Medications | Hormonal treatments that may help in reducing symptoms or preventing recurrence. |
| Watchful Waiting | Monitoring the polyps if they are not causing symptoms or complications. |
Adenomyosis: Symptoms and Management
Adenomyosis is a health issue where the inner uterus lining grows into its muscular wall. This condition leads to symptoms like severe pain in the pelvic area, heavy bleeding during menstruation, and long-lasting periods. It’s important to tell the difference between adenomyosis and endometriosis, as they require different treatments even though they seem similar.
How Adenomyosis Differs from Endometriosis
Unlike endometriosis, adenomyosis happens directly in the uterine wall. Endometriosis, on the other hand, occurs when similar tissue grows outside the uterus. The pain from adenomyosis gets worse during menstrual periods. Sometimes doctors confuse it with endometriosis because the symptoms are alike. Knowing the distinction helps in getting the right treatment.
Treatment Approaches for Adenomyosis
Treating adenomyosis depends on the needs of the individual. There are several common methods:
- Hormonal therapies: Birth control pills or hormonal IUDs can help regulate bleeding and alleviate pain.
- Pain relief medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce pain and discomfort.
- Surgical options: Hysterectomy may be considered for severe cases where other treatments fail to provide relief.
For the best advice on managing adenomyosis, talking to healthcare professionals is crucial. They can suggest treatments based on each case. Early treatment can greatly help improve life quality for those dealing with adenomyosis.
Hormonal Imbalances and Their Effect on the Uterine Lining
Hormonal imbalances have a big impact on the uterine lining’s health. Estrogen and progesterone are key for a healthy endometrial environment. If these hormones are off balance, it can cause problems with the uterine lining.
Too much estrogen can lead to a thick uterine lining, known as endometrial hyperplasia. This condition can cause heavy and abnormal bleeding. It can really interfere with daily life. Not enough progesterone means the lining won’t shed as it should. This makes bleeding issues even worse.
Stress and not eating well can also throw hormones off balance. Stress raises cortisol, which messes with hormone levels and reproductive functions. Eating right, with plenty of essential nutrients, can help balance hormones. This supports a healthier uterine lining.
Tackling hormonal imbalances involves changing lifestyles, diet, and sometimes seeking medical help. Understanding these factors lets women take steps toward better endometrial health.
Managing Endometrial Health in Women with PCOS
Women with PCOS have unique challenges in keeping their endometrial health in check. Knowing how to handle these challenges with lifestyle changes and medical support is key. This can greatly improve their well-being.
Diet and Lifestyle Changes for Better Health
Making certain lifestyle changes is critical for better endometrial health. Leading with a balanced diet and staying active are essential steps. Here’s what to include:
- Incorporating a variety of fruits and vegetables
- Opting for whole grains instead of refined grains
- Including lean proteins, such as fish and poultry
- Limiting processed foods and sugars
Staying active helps in weight management, which is vital for hormonal balance. It boosts mood and cuts stress, too. Using stress relief methods like yoga or meditation also supports mental and endometrial health management.
Medical Interventions Available
Besides lifestyle changes, there are medical options to help women with PCOS. Here are some choices:
| Intervention | Description | Potential Benefits |
|---|---|---|
| Hormonal Treatments | Use of birth control pills to regulate menstrual cycles | Reduces symptoms of PCOS and improves endometrial health |
| Metformin | Medication that improves insulin sensitivity | Aids weight management and may restore ovulation |
| Fertility Treatments | Medications like clomiphene for ovulation induction | Supports women trying to conceive |
Combining medical treatments with lifestyle changes leads to better endometrial health outcomes. Continuous research is expanding our understanding of PCOS and its effects on the uterus. For further information, check out this resource.
Conclusion
When we look closely at endometrial health, especially with PCOS, we see how vital it is to focus on this area of women’s health. The summary shared here shows why it’s important to know about conditions like endometriosis, uterine fibroids, and hormone issues. These can affect not just how we feel physically but also our reproductive health.
It’s key to take steps early to handle these issues. Women should consider different ways to manage PCOS. This can range from changing what they eat to seeking medical help. Getting advice from healthcare providers is crucial in dealing with these complicated health challenges, which helps lower the risk of endometrial problems.
Learning that a lot of women of childbearing age have endometriosis shows the importance of knowing more and diagnosing it early. The research at NCBI’s comprehensive resource points out why. With the right knowledge and healthcare support, women can stand up for their health. This helps them make smart choices for better reproductive health.