About 70% of women with PCOS face endometrial issues during their lives. Endometrial Hyperplasia is a big concern for those with PCOS. It’s due to hormonal imbalances that increase the risk of abnormal bleeding and precancerous conditions.
Early intervention can improve health outcomes. Recognizing endometrial hyperplasia early lets women manage their health better. For more details on PCOS and endometrial health, read this comprehensive review.
Key Takeaways
- Endometrial hyperplasia is common in PCOS women.
- Hormonal imbalances are a major cause of this condition.
- Abnormal bleeding may indicate endometrial hyperplasia.
- Early detection is key for healthy uterine function.
- Understanding PCOS helps in making informed health decisions.
Understanding PCOS and Its Complications
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that affects women of childbearing age. It’s important to know the symptoms of PCOS, which include irregular periods, lots of hair growth, and gaining weight. These symptoms can greatly impact a woman’s life.
People with PCOS face several complications of PCOS. Hormonal imbalances can cause insulin resistance. This condition increases the risk of type 2 diabetes. Infertility is also a major issue due to disrupted ovulation. Furthermore, there’s a link between PCOS and endometrial hyperplasia. Understanding these health risks is vital. Early medical help can reduce these dangers, especially for those with irregular periods. For further reading, visit the study on PCOS and endometrial health.
About 70% of women with PCOS have endometrial problems. This makes monitoring endometrial health important. Endometriosis and uterine fibroids can develop due to hormone changes. Recognizing these connections is key for early detection. Proper care can improve health outcomes for those affected. Being proactive about health is crucial. Learn more at resources on managing endometrial health.
The Importance of Recognizing Endometrial Hyperplasia
Endometrial hyperplasia means the uterine lining gets too thick. It often happens due to hormonal imbalances. It’s crucial for the health of women, especially those with PCOS complications.
This condition, if ignored, can lead to serious issues. The worst-case scenario is it turning into endometrial cancer.
It’s vital to have regular health checks. They help catch any problems early. Knowing about uterine health helps women get help faster, which can lead to better health outcomes.
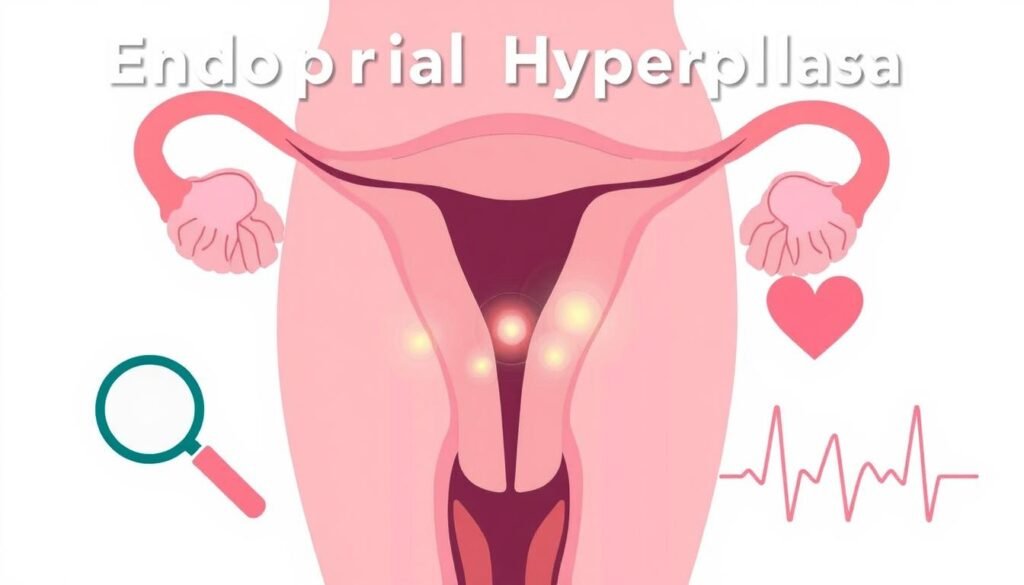
Being aware of uterine health helps women notice any unusual changes. This means they can talk to doctors sooner about any worries. Educating women about endometrial hyperplasia is a big step towards improved reproductive health.
What is Endometrial Hyperplasia?
Endometrial hyperplasia means there are too many cells in the uterus’s inner lining. It’s important to know about it to understand the risks and treatments. There are different types that doctors look at.
Definition and Types of Endometrial Hyperplasia
The endometrial hyperplasia definition splits it into simple and complex categories. Simple hyperplasia hardly leads to cancer, with a risk of less than 5%. Complex hyperplasia, though, might more likely turn into cancer, needing close watch and care.
Symptoms and Warning Signs
Knowing the symptoms of endometrial hyperplasia helps catch it early. Some common signs include:
- Abnormal bleeding during periods, which can be heavier
- Periods that go on for longer than a week
- Spotting between periods
- Bleeding after menopause
Seeing these warning signs means you should get checked out soon. Acting on abnormal bleeding issues can lower the risks that come with this condition.
| Type of Hyperplasia | Cancer Risk |
|---|---|
| Simple Hyperplasia | Less than 5% |
| Complex Hyperplasia | Higher risk of cancer |
Link Between PCOS and Uterine Lining Thickening
Polycystic ovary syndrome (PCOS) deeply affects women’s hormonal health. It leads to various issues. A main problem is uterine lining thickening. This happens because of hormonal imbalances caused by PCOS. Knowing how these imbalances lead to troubles is key for managing them well.
How Hormonal Imbalances Contribute
The hormonal shifts seen with PCOS, like less progesterone and more estrogen, are crucial. Estrogen plays a big role in making the endometrial lining grow. Without enough progesterone, this growth can go unchecked. This can cause the lining to thicken too much, which leads to more severe problems.
Estrogen Dominance and Its Role
PCOS often leads to a condition called estrogen dominance. This is when estrogen and progesterone are out of balance. It makes women with PCOS more likely to face issues like endometrial hyperplasia. If not handled, this imbalance can increase the chances of getting endometrial cancer. Women need to keep an eye on their hormonal health. Understanding this link is crucial to lower risks related to the uterus.
Abnormal Uterine Bleeding: A Common Indication
Abnormal uterine bleeding is a key sign of issues like endometrial hyperplasia. Spotting the signs early is crucial for effective endometrial health management. It’s vital for women with abnormal bleeding to watch their menstrual cycles.
Noticing unusual bleeding early helps with timely diagnosis and treatment.
Identifying Abnormal Uterine Bleeding
Abnormal bleeding has several signs, such as:
- Heavy menstrual bleeding
- Bleeding between periods
- Postmenopausal bleeding
Understanding these symptoms is important. Tracking cycles with apps or journals can help. This makes it easier for doctors to accurately assess conditions.
When to Seek Medical Attention
It’s critical to know when to get medical help for abnormal bleeding. Immediate consultation should happen if you notice:
- Bleeding lasting longer than seven days
- Soaking through one or more pads or tampons every hour for several consecutive hours
- Sudden changes in menstrual patterns
Getting help quickly can avoid complications and improve understanding of health needs. For more insights on managing these symptoms, check here.
Diagnosing Endometrial Hyperplasia
Finding out if someone has endometrial hyperplasia is very important. This process starts with a good look at the patient’s health history. A doctor examines them physically. They pay special attention to the patient’s periods and any signs that the womb’s lining might have issues.
To confirm if a patient has endometrial hyperplasia, a doctor often does an endometrial biopsy. This test takes a tiny bit of tissue from the womb’s lining. This sample is then checked in a lab. The biopsy results show if hyperplasia is present and what type it is. This helps the doctor decide on the best treatment. Ultrasounds also help by showing how thick the lining is.
Understanding that you might have endometrial hyperplasia is a key step. It leads to getting help early. Doctors use health history, a physical check, scans, and a biopsy for a correct diagnosis. This way, they can give the right treatment to those in need.