Did you know up to 70% of women with Polycystic Ovary Syndrome (PCOS) face insulin resistance? This fact highlights the need for good management in those dealing with PCOS. Regular Blood Sugar Testing is key for keeping an eye on and dealing with insulin resistance. It lets individuals with PCOS manage their health better. By knowing and watching their blood sugar, they can significantly better their PCOS care and lower the risk of related health issues.
Understanding the link between insulin resistance and PCOS is crucial. It can lead to better health and a higher quality of life. Regular Blood Sugar Testing not only gives insights into metabolic health but also helps guide diet and lifestyle changes. These are crucial for PCOS control. By focusing on managing blood sugar, people can lessen the risks of diabetes and heart diseases. They take a proactive stand in their health. Learn about insulin resistance in PCOS and why blood sugar monitoring is important in this guide: read more.
Key Takeaways
- Regular Blood Sugar Testing is essential for managing insulin resistance in PCOS.
- Studies show that 70% of women with PCOS may experience insulin resistance.
- Monitoring blood glucose levels helps individuals make informed lifestyle choices.
- Effective management can reduce the risk of diabetes and cardiovascular diseases.
- Empowered patients can take control of their health through education and regular testing.
Understanding PCOS and Insulin Resistance
Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder. It affects many women in their childbearing years. Key to managing it is knowing its symptoms and causes. Women may face various issues, including irregular periods, weight gain, and more body hair.
What is PCOS?
The American College of Obstetricians and Gynecologists describes PCOS as a hormonal imbalance leading to several health problems. Symptoms often include menstrual irregularities and metabolic issues. Understanding these signs early contributes to better treatment and outcomes.
The Link Between Insulin Resistance and PCOS
An important part of managing PCOS is dealing with insulin resistance. Studies show nearly 70% of women with PCOS struggle with insulin issues. Insulin resistance can worsen metabolic problems. Therefore, keeping an eye on blood sugar is crucial. It helps make smart choices about lifestyle and care. To learn more, one can look into essential steps to prevent complications.
| Symptom | Frequency in PCOS Patients |
|---|---|
| Irregular Periods | 70% – 80% |
| Excess Androgen Levels | 50% – 70% |
| Insulin Resistance | Up to 70% |
The Importance of Regular Blood Sugar Testing
Checking blood sugar regularly is key in managing diabetes well. It’s very important for those with insulin resistance, like in PCOS cases. By checking your blood sugar often, you get timely information. This helps you make smart choices for your health.
How Regular Blood Sugar Testing Helps
By testing your blood sugar often, you can:
- Notice unusual blood sugar levels quickly.
- Change what you eat based on your blood sugar readings.
- See if your medicine or insulin is working.
- Understand how changing your lifestyle can affect your blood sugar levels.
Key Metrics to Monitor
Some key numbers help track blood sugar effectively. Watching these helps you manage diabetes over the long term:
| Metric | Normal Range | Implication |
|---|---|---|
| Fasting Blood Sugar | 70-100 mg/dL | Tells you your starting blood sugar level after not eating. |
| A1C Level | Below 5.7% | Gives an average of your blood sugar control over 2-3 months. |
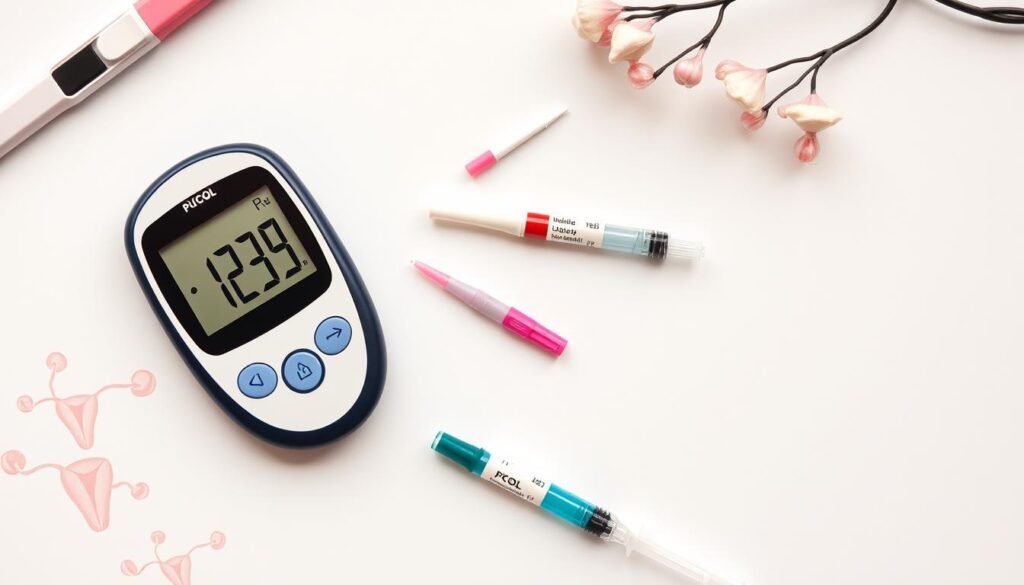
Blood Sugar Testing Methods
When managing diabetes, it’s crucial to know the different ways to test blood sugar. There are several methods to choose from, each with its benefits. Two popular methods are Self-Monitoring Blood Glucose (SMBG) and Continuous Glucose Monitoring (CGM). They help users understand their glucose levels better.
Self-Monitoring Blood Glucose (SMBG)
With SMBG, you use a blood glucose meter for testing. You do this by pricking your finger. This method helps you make quick decisions about insulin and food. By doing regular blood sugar testing with SMBG, you can track your levels at key times. For example, before and after eating. It requires testing several times a day, but it helps you manage diabetes actively.
Continuous Glucose Monitoring (CGM)
CGM is an advanced way to monitor glucose. It involves placing a sensor under your skin to track levels all the time. It gives you live data, making it easy to see highs and lows. CGM devices are more expensive than regular meters but provide constant glucose level info. Using CGM alongside SMBG gives a complete picture of your glucose trends. This helps manage diabetes better.
For more information, visit resources that explain blood sugar testing in detail. Check out this guide for example. Knowing these methods is key to good glucose control and avoiding complications.
Implementing a Diabetes Management Plan
Crafting a diabetes management plan allows people to reach their health goals. It focuses on strategies that meet personal needs, leading to improved health.
Personalized Health Goals
Setting personal health goals is key in managing diabetes. By identifying clear objectives, individuals can monitor their success. Goals might include achieving a healthy A1C level, increasing physical activity, or making better food choices.
- Maintaining a specific A1C level
- Engaging in regular physical activity
- Improving dietary choices and monitoring carbohydrate intake
Goals should match one’s health status and aspirations. Regular checks ensure these aims stay relevant, guiding toward the intended results.
Integrating A1C Testing Into Your Routine
A1C tests are vital for tracking blood sugar over months. Adding these tests to regular health check-ups gives valuable insight for managing diabetes. Steps include:
- Scheduling regular A1C tests as recommended.
- Discussing results to tweak the management plan.
- Understanding A1C’s role in overall health and diabetes care.
Doing this helps update health goals timely, enhancing management effectiveness.

| A1C Level (%) | Blood Sugar Average (mg/dL) | Management Action |
|---|---|---|
| Below 5.7 | Less than 110 | Maintain current management plan |
| 5.7 – 6.4 | 110 – 140 | Review diet and activity levels |
| 6.5 and above | 140 and above | Consider alternative management options |
Diet and Healthy Eating for PCOS
For those managing PCOS, eating well is key. It helps control blood sugar. This boosts overall health for women with insulin resistance.
Making smart food choices eases PCOS symptoms. It does this by keeping blood sugar levels stable.
Foods to Incorporate for Blood Sugar Control
When planning a PCOS diet, certain foods are beneficial:
- Whole grains such as quinoa, brown rice, and oats.
- Lean proteins like chicken breast, turkey, and legumes.
- Non-starchy vegetables including spinach, broccoli, and bell peppers.
- Healthy fats from sources like avocados, nuts, and olive oil.
These foods don’t cause big insulin spikes. Eating them regularly helps maintain steady blood sugar. This leads to better health.
Meal Planning Tips for Insulin Resistance
Meal planning is crucial for PCOS management. Here are useful tips:
- Create a weekly meal plan to ensure balanced nutrition.
- Prep meals in advance to avoid impulsive eating choices.
- Track macronutrient intake to maintain a healthy balance.
- Include snacks that consist of protein and fiber to aid in blood sugar management.
These strategies improve eating habits. They promote blood sugar control and enhance health.

| Food Type | Recommended Choices | Benefits |
|---|---|---|
| Whole Grains | Quinoa, brown rice, whole oats | Low GI; maintains steady energy |
| Lean Proteins | Chicken breast, fish, legumes | Builds muscle; keeps you full |
| Non-Starchy Vegetables | Spinach, broccoli, cauliflower | Rich in nutrients; low in calories |
| Healthy Fats | Avocados, nuts, olive oil | Supports hormone balance; aids satiety |
Exercise Routine for Managing PCOS
Being active is key in managing Polycystic Ovary Syndrome (PCOS) symptoms. A good workout plan can make your body more sensitive to insulin. This helps keep your blood sugar in check and boosts your health. It’s important to know which exercises are best and how to stick to your routine.
Types of Exercise Beneficial for Insulin Sensitivity
Aerobic and resistance training both play a big part in improving insulin sensitivity. Here are some top activities:
- Walking: Walking is easy to do every day and really beneficial.
- Running or jogging: These are more intense but great for your heart.
- Swimming: Perfect for those with joint problems because it’s low-impact.
- Weight training: Building muscle is crucial as it improves your metabolism.
Creating a Sustainable Exercise Plan
Making a exercise plan you can stick to is important. Here’s how to do it:
- Set goals that are achievable based on what you like and your current fitness level.
- Try different activities to keep things fun and interesting.
- Work out at the same times each week to form a routine.
- Keep track of your progress to stay motivated and tweak things as you go.
To learn more about managing PCOS and its metabolic risks, check out the dietary changes and goals discussed here.
Managing Hypoglycemia and Hyperglycemia
Learning to manage blood sugar is key for those with PCOS and similar conditions. Managing very low or high blood sugar takes careful effort to keep levels right. Being aware and taking action early makes handling blood sugar dips and spikes easier.
Preventing Hypoglycemia During Treatment
To stop hypoglycemia, watching what you eat and managing insulin right is crucial. Some ways to help include:
- Eating regular, balanced meals to keep blood sugar steady.
- Having fast-acting sugar sources like glucose tablets ready if needed.
- Talking with a healthcare pro to plan meals and meds.
Recognizing Signs of High Blood Sugar
Knowing the signs of too high blood sugar helps you act fast to avoid worse problems. Signs to watch for include:
- Frequent urination
- Increased thirst
- Fatigue or weakness
- Blurred vision
Checking blood sugar daily helps catch issues early. Learning more about handling both low and high blood sugar is vital for better health over time.
| Condition | Symptoms | Prevention Strategies |
|---|---|---|
| Hypoglycemia | Dizziness, shaking, sweating | Regular meals, carry sugar sources |
| Hyperglycemia | Frequent urination, increased thirst | Monitor blood sugar, adjust medication |
Insulin Therapy and Its Role in PCOS
Insulin therapy is a key approach for managing PCOS, especially insulin resistance. It helps balance metabolism and improve health outcomes.
Understanding Insulin Therapy Options
There are different insulin therapy options. Patients might find:
- Long-acting insulins – They release insulin slowly, keeping blood sugar stable all day.
- Rapid-acting insulins – These work quickly, controlling blood sugar spikes after meals.
- Insulin pumps – This technology offers constant insulin delivery for precise control.
Each type of insulin therapy has its own purpose. The choice depends on health needs and managing insulin resistance.
When to Consider Insulin Therapy
Reasons to consider insulin therapy include:
- Persistent high blood sugar despite changing lifestyle
- Signs of severe insulin resistance
- Having had gestational diabetes, which raises the risk of type 2 diabetes
Talking with healthcare experts is vital for personalized treatment. They help decide if insulin therapy is needed, based on health.
| Insulin Therapy Type | Usage | Benefits |
|---|---|---|
| Long-acting insulins | Daily control of blood sugar | Steady insulin levels throughout the day |
| Rapid-acting insulins | Post-meal blood sugar control | Minimizes spikes after eating |
| Insulin pumps | Continuous insulin delivery | Customizable dosage based on needs |
Conclusion
Regular blood sugar tests are key in managing PCOS, especially with insulin resistance. It lets people spot trends and make smart health choices. This leads to better health results. Diet, exercise, and medical help are very important in this process.
Being proactive helps people take charge of their health. It also encourages healthy lifestyle changes. Regular blood sugar checks help meet health goals and boost well-being. Talking to doctors and looking into test methods is crucial. Resources like blood glucose testing techniques are very helpful.
Adding blood sugar tracking to daily life is essential for those with PCOS. It helps manage insulin resistance better. By learning more and focusing on self-care, people can improve their health. This leads to a happier life.