The Centers for Disease Control finds that 6% to 12% of women of childbearing age in the US are affected by Polycystic Ovary Syndrome (PCOS). This disorder leads to issues like irregular periods and excess hair growth. But it’s also closely linked to insulin resistance, affecting a woman’s health in many ways.
About 65% to 70% of women with PCOS struggle with this hormonal issue. It raises their risk for serious problems like Type 2 diabetes and heart disease. In fact, having PCOS makes a woman four to nine times more likely to get Type 2 diabetes. More than half are diagnosed by the time they turn 40.
It’s critical to understand how PCOS and insulin resistance interact. This knowledge can improve treatment and help women achieve better reproductive health.
Key Takeaways
- PCOS affects 6% to 12% of reproductive age women in the US.
- Up to 70% of women with PCOS have insulin resistance.
- Women with PCOS are four to nine times more likely to develop Type 2 diabetes.
- Over half of women with PCOS will be diagnosed with Type 2 diabetes by age 40.
- Lifestyle changes can effectively help manage symptoms of PCOS and insulin resistance.
- Routine blood tests are recommended to check for insulin resistance in women with PCOS.
Introduction to PCOS
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder among women of childbearing age. It involves symptoms like hormonal imbalances and small cysts on the ovaries. Understanding PCOS is key to managing its impact on health.
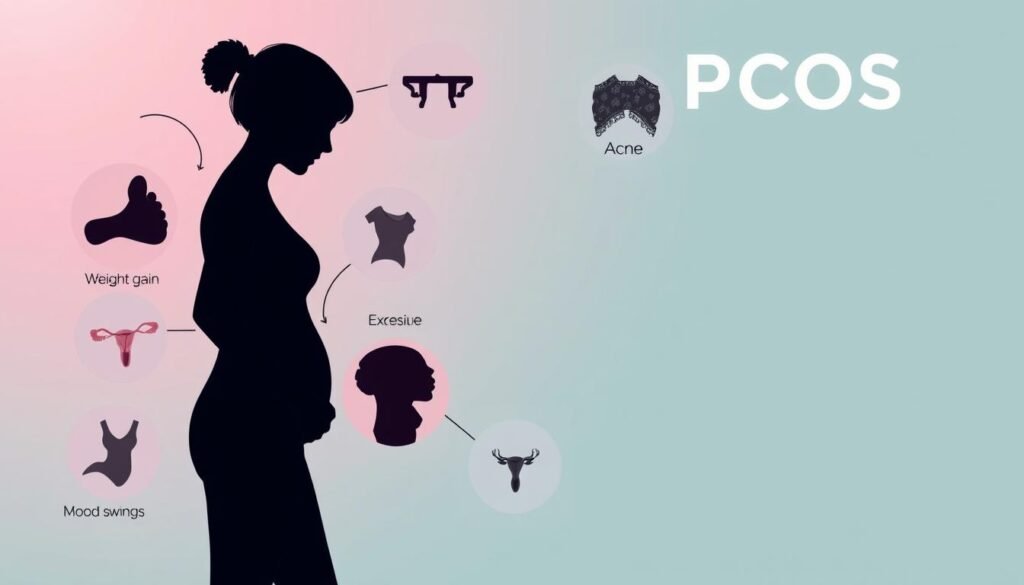
Definition and Common Symptoms
PCOS symptoms vary from one person to another, so it’s important to know the early signs. Common symptoms include:
- Irregular menstrual periods
- Weight gain or obesity
- Excess hair growth or hirsutism
- Acne and oily skin
- Infertility issues
Knowledge of these symptoms is essential for women to get timely help. Studies show PCOS affects about 5% to 18% of women during their reproductive years. Spotting it early is crucial to manage symptoms and avoid future health issues like diabetes and heart disease.
The Importance of Early Diagnosis
Getting diagnosed with PCOS early is key for effective management and avoiding long-term health problems. Women with PCOS are more likely to have insulin resistance and metabolic syndrome. Knowing about these risks helps in taking steps to protect hormonal health.
Early intervention can also reduce the risk of serious complications. For women with a family history of PCOS, early diagnosis is especially important. It can provide family support and a better understanding of the condition.
What is Insulin Resistance?
Insulin resistance is important when we talk about metabolic disorders, especially with Polycystic Ovary Syndrome (PCOS). Insulin helps manage blood sugar, helping glucose enter our cells. But with insulin resistance, cells don’t react properly to insulin. This leads to too much glucose in the blood, known as hyperglycemia. It’s a problem that can impact health beyond just PCOS.
Understanding Insulin and Its Role
The pancreas makes insulin, which helps control blood sugar levels. It helps cells absorb glucose for energy. But if you have insulin resistance, this system doesn’t work right.
The body tries to fix this by making more insulin, leading to high insulin levels. This can make PCOS symptoms worse, like weight gain and irregular periods. It can also lead to other health problems.
How Insulin Resistance Develops
Lifestyle factors, like diet and exercise, really matter for insulin resistance, especially in PCOS. Being overweight and certain hormones also play a big role. Studies show 65 to 70% of women with PCOS have insulin resistance.
This rate goes up to 70 to 80% for obese women with PCOS. This is why it’s crucial to keep an eye on insulin sensitivity. Healthier eating and regular exercise can make a big difference in insulin sensitivity and health.
It’s key to understand how insulin works with glucose, especially for managing PCOS. For more info on insulin resistance and PCOS, check out this informative resource.
| Factor | Impact on Insulin Resistance |
|---|---|
| Genetic Predisposition | Higher likelihood of developing insulin resistance |
| Obesity | Increased risk; 70-80% of obese women with PCOS |
| Poor Diet | Can worsen insulin sensitivity |
| Lack of Exercise | Negatively impacts glucose metabolism |
Exploring the Connection Between PCOS and Insulin Resistance
The link between PCOS and insulin resistance is key to a woman’s health. It affects hormonal balance and reproductive functions. Understanding this connection helps tackle PCOS.
How Insulin Resistance Affects Hormonal Balance
Insulin resistance can mess with hormonal balance in women with PCOS. High insulin levels can increase androgens, or male hormones. This imbalance can cause hair growth issues and skin changes.
It’s crucial for patients to get how insulin impacts their health.
Impact on Ovarian Function and Menstrual Cycle
Insulin resistance also affects ovarian function and menstrual cycle regularity. It can stop follicle development, causing menstrual problems like oligomenorrhea or anovulation. Many women with PCOS face these issues.
Knowing about insulin’s effects is key for managing PCOS. It shows why focused treatments and lifestyle changes are needed for better health.
Symptoms Associated with PCOS and Insulin Resistance
The diverse symptoms of PCOS and signs of insulin resistance greatly affect women’s lives. Knowing these symptoms helps with earlier diagnosis and treatment. This empowers women to get the right help.
Common Symptoms of PCOS
PCOS symptoms vary widely among women. Some common ones are:
- Irregular or no menstrual periods
- Hirsutism, or too much hair in unwanted spots
- Acne and oily skin
- Weight gain or trouble losing weight
- Acanthosis nigricans, which are dark skin patches
Signs of Insulin Resistance
It’s vital for women with PCOS to recognize insulin resistance signs. Some common ones are:
- Constant cravings for sweet foods
- Needing to urinate often
- Feeling tired or without energy all day
- Feeling more hungry, especially after eating
As many as 80% of women with PCOS may have insulin resistance. Knowing the signs of insulin resistance helps with early intervention and treatment.
For more about the symptoms of PCOS and what they mean, check out this informative resource. Education is key, as many women don’t know their symptoms. This makes learning about PCOS vital for good health management.
Causes of PCOS and Insulin Resistance
The causes of PCOS are still being extensively studied. Many factors can lead to its development. Genetics and lifestyle are key in determining risk. Knowing about these can help people take steps to manage or prevent PCOS.
Genetic Factors
Genetics play a big role in PCOS risk. If PCOS runs in the family, you might be more likely to get it. Some genes could make you more prone to insulin issues, making PCOS symptoms worse. Understanding these genetic links helps in finding the right treatment early.
Knowing your family’s health history can point out preventive steps for PCOS.
Lifestyle and Environmental Influences
How you live can strongly impact PCOS symptoms. Bad eating habits, not exercising, and being overweight can make insulin problems worse. This can lead to more health issues. Yet, staying active and eating well can cut the risk of serious diseases like diabetes and heart problems.
Health experts focus on lifestyle changes to help with PCOS. For more tips, see these insightful resources. Also, learn about PCOS and metabolic risks at this informative site.
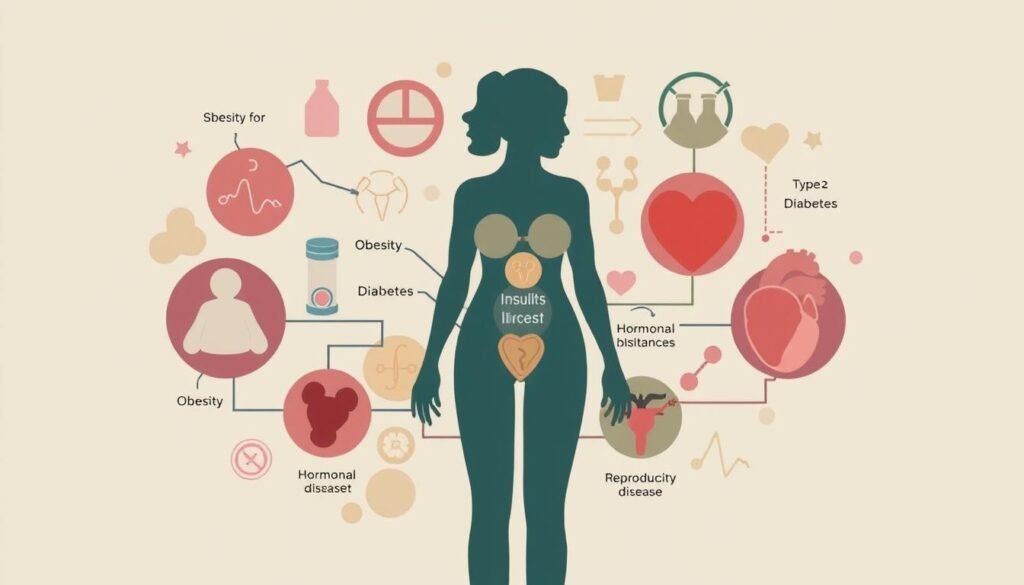
Health Risks Linked to PCOS and Insulin Resistance
Understanding the health risks linked to PCOS is important. This condition can lead to many long-term health issues. A major concern is the higher risk of type 2 diabetes in women with PCOS. Many of them face insulin resistance, raising their diabetes risk over time.
Increased Risk of Type 2 Diabetes
Studies show that more than half of women with PCOS will face type 2 diabetes by age 40. Insulin resistance is common among them, affecting their body’s glucose processing. This condition spikes their blood sugar levels. Therefore, checking for insulin resistance early is key.
Cardiovascular Health Concerns
PCOS also increases the risk of cardiovascular disease. Women with PCOS often have higher blood pressure and bad lipid levels. The chance of heart disease goes up as they age, especially if they are obese. Making lifestyle changes, like eating better and exercising, can help improve heart health.
| Health Risks | Impact Level | Preventive Measures |
|---|---|---|
| Type 2 Diabetes | High | Regular screening and lifestyle changes |
| Cardiovascular Disease | Moderate to High | Healthy diet and exercise |
| Long-term Health Complications | High | Early diagnosis and management |
Diagnosing PCOS and Insulin Resistance
Diagnosing PCOS the right way is key to help manage it. Healthcare pros use several tests to check if someone has PCOS and if they’re insulin resistant too. Knowing how to diagnose it correctly is super important. It helps patients get the care they need.
Common Diagnostic Tests
Doctors use different tests to find out if someone has PCOS. They look at hormone levels, how the body processes sugars, and check the ovaries. Some important tests are:
- Hormone tests from a blood sample
- Sugar tests to see how the body uses insulin
- Checks of the reproductive organs
- Scans of the ovaries looking for cysts
These tests help doctors understand what’s going on. This way, they can start helping the patient sooner.
Criteria for Diagnosis
To diagnose PCOS, patients must meet at least two specific criteria:
- Having irregular periods
- High levels of androgens, which might cause more hair or acne
- Ovaries that have many cysts, seen in an ultrasound
Knowing these points helps in diagnosing PCOS. It also helps spot insulin resistance. Awareness of risk factors, like being overweight, also helps catch it early.
Managing PCOS and Insulin Resistance
For PCOS and insulin resistance, a mix of dietary changes, exercise, and medicine is key. Every part is important for better health and easing symptoms of this issue.
Dietary Changes and Nutrition Tips
A good diet is crucial for PCOS management. Since 50% to 75% of people with PCOS have insulin resistance, eating right is critical. Foods that boost insulin sensitivity are a focus. The Mediterranean diet is popular. It includes:
- Omega-3 rich fish
- Non-starchy vegetables
- Whole grains
- Legumes
- Low-sugar beverages
- Olive oil
Staying hydrated is essential. Water and unsweetened drinks are best. It’s wise to limit foods causing inflammation like fried items, red meat, and sugary drinks. Eating small, nutritious meals regularly maintains stable blood sugar.
Exercise and Lifestyle Modifications
Exercise is a big help in PCOS management. It supports weight loss and boosts insulin sensitivity, both are vital. Changes in lifestyle can lead to better health outcomes like more regular ovulation and improved metabolism. Combining aerobic and strength exercises is beneficial. This improves overall health and the exercise impact on insulin resistance.
Medications for Management
Sometimes, drugs like metformin are used for better insulin sensitivity and hormone balance in PCOS. Metformin can help lose weight, reduce blood sugar levels, and enhance metabolic health. However, it might cause stomach issues. It’s important to follow the doctor’s advice on how to use this medication.

PCOS and Insulin Resistance: Treatment Options
Polycystic Ovary Syndrome (PCOS) presents various challenges that need careful handling. Discovering the right treatment can improve life and manage symptoms well. Different medicines are discussed to meet personal needs.
Overview of Medications
Hormonal contraceptives help with menstrual cycles and issues like hirsutism and hair loss. Metformin is good for lowering insulin and sugar levels in PCOS patients. Letrozole is effective in inducing ovulation, often used off-label for this.
If pills don’t work, injections called gonadotrophins may help with conception.
Alternative Therapies and Supplements
Alternative therapies add extra support in dealing with PCOS and insulin resistance. Inositol supplements can improve ovarian function and health. Making changes in lifestyle like exercising and mindful practices is very helpful.
Losing just 5% weight can make a big difference. It’s key to keep a healthy Body Mass Index (BMI). Eating right is crucial, including cutting back sugar to less than 45 grams daily.
Conclusion
Understanding the link between polycystic ovary syndrome (PCOS) and insulin resistance is key. About 35–80% of women with PCOS have insulin resistance. This can lead to serious health issues like metabolic syndrome and type 2 diabetes.
The importance of knowing the symptoms and risks of PCOS is huge. Timely diagnosis and comprehensive management are crucial for better health in women with PCOS. Recognizing insulin resistance signs and making positive life changes are big steps towards health.
A multifaceted approach is needed to manage PCOS. This includes diet changes and exercise. It helps people take an active role in their health.
Empowering women with knowledge about PCOS is vital. It encourages them to take a proactive approach to their health. As research evolves, staying informed helps control one’s well-being.
Continued awareness and education let women handle their PCOS with confidence. This reduces the risk of chronic conditions from untreated insulin resistance.